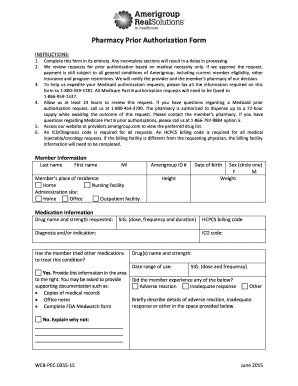
Get the free medco prior authorization form
Show details
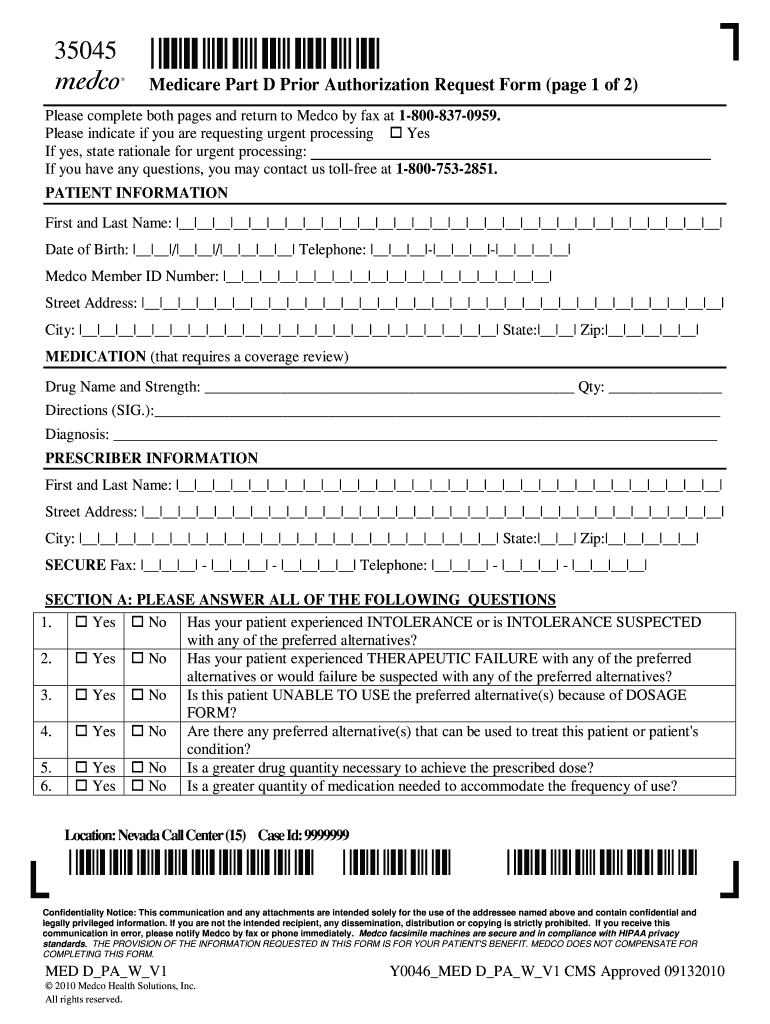
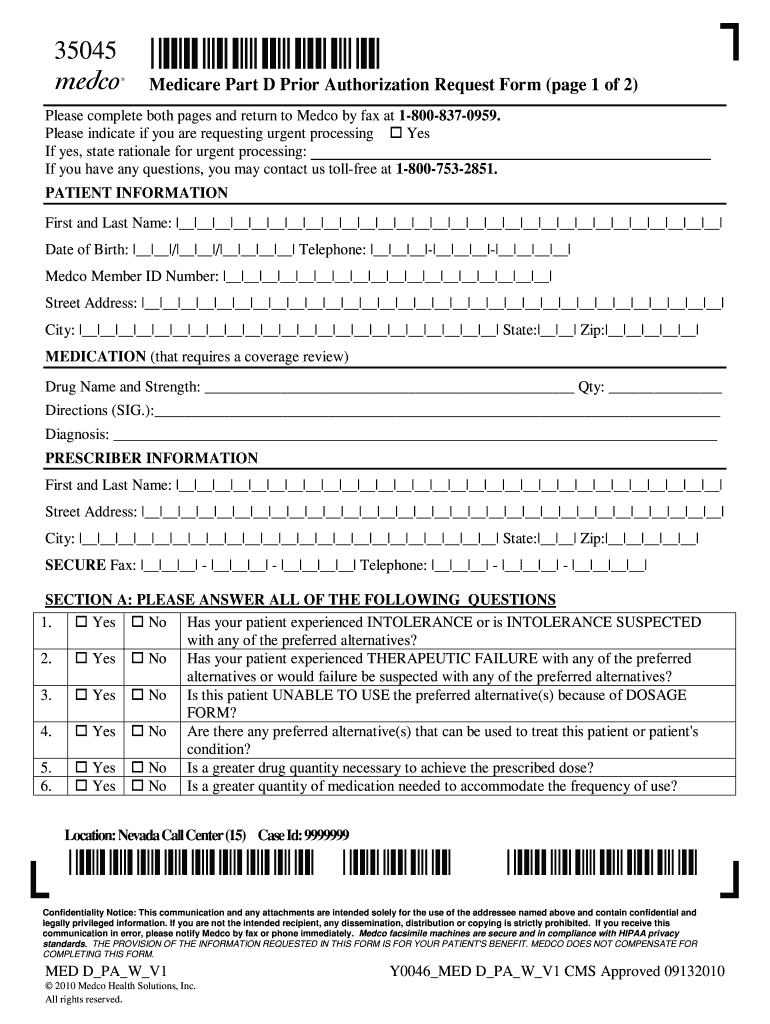
35045 35045* Medicare Part D Prior Authorization Request Form (page 1 of 2) Please complete both pages and return to Medico by fax at 1-800-837-0959. Please indicate if you are requesting urgent processing
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign medco express scripts prior authorization form

Edit your medco health prior authorization form form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.

Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.

Share your form instantly
Email, fax, or share your medco prior authorization forms form via URL. You can also download, print, or export forms to your preferred cloud storage service.
Editing medco prior auth form online
Follow the steps down below to benefit from the PDF editor's expertise:
1
Create an account. Begin by choosing Start Free Trial and, if you are a new user, establish a profile.
2
Upload a file. Select Add New on your Dashboard and upload a file from your device or import it from the cloud, online, or internal mail. Then click Edit.
3
Edit medco prior authorization form. Replace text, adding objects, rearranging pages, and more. Then select the Documents tab to combine, divide, lock or unlock the file.
4
Save your file. Select it from your records list. Then, click the right toolbar and select one of the various exporting options: save in numerous formats, download as PDF, email, or cloud.
pdfFiller makes working with documents easier than you could ever imagine. Register for an account and see for yourself!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out medco pharmacy prior authorization form

To fill out the medco prior authorization, follow these steps:
01
Gather all necessary information and documents such as patient demographics, medical history, and prescription details.
02
Complete the medco prior authorization form accurately, providing all requested information.
03
Attach any supporting documentation, such as medical records or test results, that may be required for the authorization.
04
Review the filled-out form for any errors or missing information before submitting it.
05
Submit the completed medco prior authorization form to the appropriate department or organization for review and approval.
Medco prior authorization is typically required for individuals who meet specific criteria set by the insurance provider or pharmacy benefit manager. These criteria may include specific medications, dosage amounts, alternative therapies, or certain medical conditions. It is essential to check with your insurance company or pharmacy benefit manager to determine if prior authorization is required for your prescription. Failure to obtain prior authorization, when necessary, may result in coverage denial or increased out-of-pocket expenses for the medication.
Fill
medco medicare part d
: Try Risk Free






People Also Ask about people also ask about medco you go to the pharmacy
What triggers a prior authorization?
The prior authorization process begins when a service prescribed by a patient's physician is not covered by their health insurance plan. Communication between the physician's office and the insurance company is necessary to handle the prior authorization.
How do I get prior authorization Express Scripts?
Your doctor can initiate the prior authorization process by calling Express Scripts toll-free at 800‑417‑8164 or by fax at 800‑357‑9577. If you plan to fill your prescription at a retail pharmacy, consider completing the prior authorization with your doctor before you go to the pharmacy.
How can I speed up my prior authorization?
Following up on prior authorizations in a timely manner can help alleviate some of the delays in obtaining an authorization and providing patient care. Create A Follow Up Plan With Your Staff. Be Methodical About Working Authorizations. Ask For An Estimated Turnaround Time For The Completion Of An Authorization.
Why does my medication need a prior authorization?
What is prior authorization? This means we need to review some medications before your plan will cover them. We want to know if the medication is medically necessary and appropriate for your situation. If you don't get prior authorization, a medication may cost you more, or we may not cover it.
Why does Adderall need prior authorization?
This is to ensure that the medication is appropriate for your treatment. It also helps to make sure it's the most cost-effective option. When prior authorization is granted, it is typically for a specific length of time. You will need to request prior authorization again if you need a refill after the timeframe passes.
Why is it so hard to get prescribed ADHD medication?
What's the cause of the shortage? Rojas: It has to do with supply chain issues and a spike in demand from adults, especially during COVID-19 when ADHD symptoms got worse for many and the drug could be prescribed online for the first time.
Our user reviews speak for themselves
Read more or give pdfFiller a try to experience the benefits for yourself
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I get medco part d?
The pdfFiller premium subscription gives you access to a large library of fillable forms (over 25 million fillable templates) that you can download, fill out, print, and sign. In the library, you'll have no problem discovering state-specific medco medicare and other forms. Find the template you want and tweak it with powerful editing tools.
Can I create an electronic signature for the to fill out the medco pocket expenses for the medication in Chrome?
Yes. By adding the solution to your Chrome browser, you can use pdfFiller to eSign documents and enjoy all of the features of the PDF editor in one place. Use the extension to create a legally-binding eSignature by drawing it, typing it, or uploading a picture of your handwritten signature. Whatever you choose, you will be able to eSign your medco provider phone number in seconds.
Can I edit medicare prior authorization form on an Android device?
Yes, you can. With the pdfFiller mobile app for Android, you can edit, sign, and share printable medical prior authorization form template on your mobile device from any location; only an internet connection is needed. Get the app and start to streamline your document workflow from anywhere.
What is medco prior authorization form?
The Medco prior authorization form is a document used by healthcare providers to obtain approval from an insurance company before a specific medication is dispensed to a patient. This form ensures that the prescribed medication is covered under the patient's insurance policy.
Who is required to file medco prior authorization form?
Typically, the healthcare provider or physician issuing the prescription is required to file the Medco prior authorization form. However, in some cases, the pharmacy may assist in this process.
How to fill out medco prior authorization form?
To fill out the Medco prior authorization form, you need to provide patient information, prescription details, the medical necessity of the medication, and any relevant clinical information or previous treatments. Ensure that all sections of the form are completed accurately and check for any specific insurer requirements.
What is the purpose of medco prior authorization form?
The purpose of the Medco prior authorization form is to ensure that certain medications are medically necessary and meet the insurance company's coverage criteria. It helps control costs and ensures that patients receive appropriate medication.
What information must be reported on medco prior authorization form?
The Medco prior authorization form must include patient identification details, prescriber information, medication name and dosage, diagnosis, treatment history, and a justification for why the prescribed medication is necessary.
Fill out your medco prior authorization form online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.
Medicare Prior Authorization Form Pdf is not the form you're looking for?Search for another form here.
Keywords relevant to express scripts prior authorization form pdf
Related to medco fax order form
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.